Introduction: Among Therapy-Related Myeloid Neoplasms (t-MNs), there are two large groups depending on the cytotoxic trigger. A first group arises after exposure to alkylating agents and / or radiation in the previous 5-10 years and it is associated with unbalanced chromosomal abnormalities, frequently with alterations in Cr 5, 7, complex karyotype and mutated TP53. The second arises after exposure to topoisomerase II inhibitors in the previous 1-5 years, and it is characterized by frequent balanced translocations and KMT2A rearrangement. In those cases with a latency time from cytotoxic exposure to T-MNs diagnosis greater than 10 years, there is doubt about whether they should be considered T-MNs or de novo leukemias.
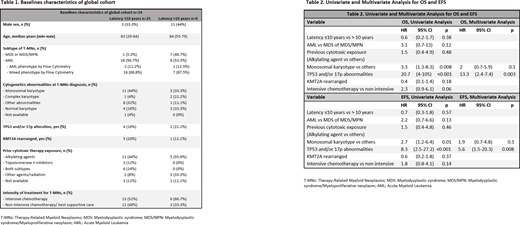
Material and methods: We performed a retrospective analysis of 34 patients with diagnosis of T-MNs treated in our center between 2013 and 2019. We have reviewed the cytogenetic alterations at diagnosis and alterations in TP53 and / or 17p and rearrangements in KMT2A. We divided the cohort into two groups based on the latency time of ≤10 years or> 10 years. The comparison between both groups was carried out using the chi2 test for qualitative variables and the t-student for quantitative variables. The Kaplan Meier method has been used for the calculation of Overall Survival (OS) and Event Free Survival (EFS) and the Cox regression model for the univariate and multivariate analysis.
Results: The median follow-up of the global cohort was 8.5 months (0-74). The median OS of the global cohort was 10 months and the EFS was 8 months. In patients with a latency time ≤10 years the median OS was 12 months vs 9 months in those with latency >10 years, with a Hazard Ratio (HR) of 0.6 [95% CI (0.2-1.7), p = 0.3] and the EFS was 7 months vs 9 months respectively [HR 0.3, 95% CI (0.3-1.8), p = 0.7]. The baseline characteristics of the population are reflected in Table 1. A similar percentage of patients with complex or monosomal karyotype at diagnosis is observed in both groups, as well as alterations in TP53 and/or 17p. In the >10-year latency subgroup, there were no patients with prior exposure to Topoisomerase II Inhibitors. Within the <10-year latency group, we divided the cohort into two groups: 1 to 5 years and 5 to 10 years of latency. No differences were found for OS [HR 1.5 95% CI (0.4-5), p = 0.4] or for EFS [HR 2.1 95% CI (0.7-6.2), p = 0.1]. A univariate analysis was performed including the characteristics reflected in Table 2. The variables with a significant HR for OS and EFS were to present a monosomic karyotype at diagnosis and alterations in TP53 and/or 17p. In the multivariate analysis, only the alterations in TP53 and/or 17p maintained a significant HR.
Conclusions: Patients with a latency time from exposure to cytotoxic therapy to the diagnosis of T-MNs > 10 years, presented cytogenetic and molecular characteristics similar to those with an exposure time ≤10 years, as well as a similar OS and EFS. Regarding the cytogenetic characteristics at diagnosis of the general cohort, patients with monosomic karyotype and especially those with TP53 and/or 17p alterations had a worse prognosis.
Garcia-Gutiérrez:Incyte:Consultancy, Other: Travel, Accommodation, Expenses, Research Funding;Novartis:Consultancy, Other: Travel, Accommodation, Expenses, Research Funding;Bristol-Myers Squibb:Consultancy, Other: Travel, Accommodation, Expenses, Research Funding;Pfizer:Consultancy, Other: Travel, Accommodation, Expenses, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal